
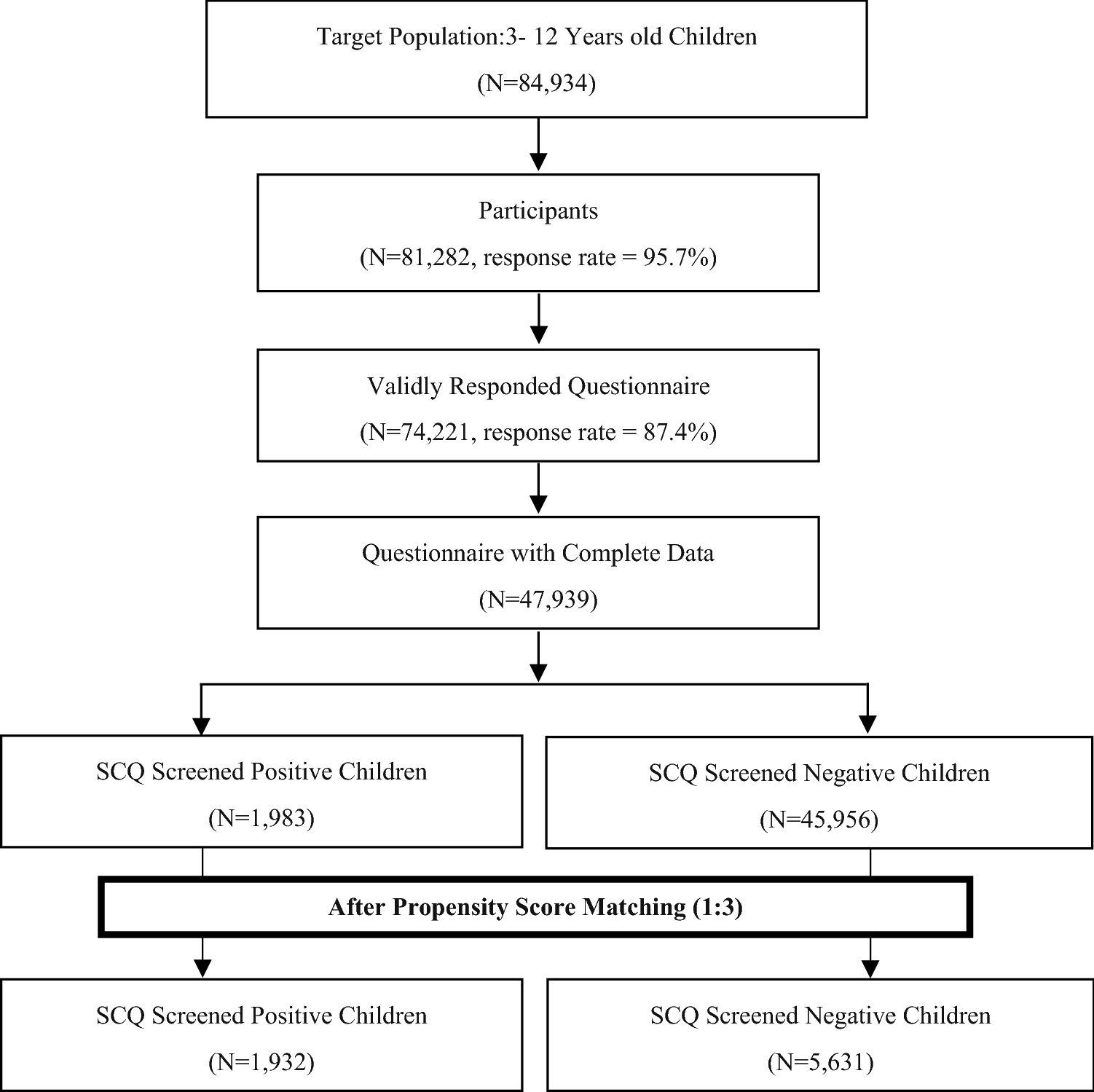
Prospective cohort studies with laboratory confirmation of infections are ideal but are often hampered by low numbers of events, particularly for outcomes such as fetal birth defects. However, these studies have a few limitations. In addition, urinary tract infections, especially pyelonephritis 26 are reported to associate with preterm birth. Even short exposures to elevated maternal body temperature have been reported to lead to cell death, vascular disruptions, and placental infarction 25. It was reported that fever has been suspected to harm the developing fetus 24. estimated that 5–10% of women, on average, report a fever in early pregnancy 23. Maternal fever is also common during pregnancy. Influenza during pregnancy has been linked to spontaneous abortion, stillbirth, and prematurity 21, 22. For instance, pregnant women are vulnerable to viral respiratory infections 19 and are found to be at high risk for influenza and related complications 17, 20. Infections are the result of infectious agents including viruses, viroids, prions, bacteria, nematodes and so on. There is also growing evidence that some infections during pregnancy may play an important role in the occurrence of adverse pregnancy outcomes and congenital anomalies 16, 17, 18. For instance, lack of maternal multivitamin use 13, maternal age, education and economic level, maternal use of drug 13, alcohol 14, and cigarettes 15 during pregnancy have all been associated with the occurrence of fetal anomalies. Throughout gestation, they are generally considered induced by the complex effects of genetic and multiple environmental risk factors 12. The mechanisms of adverse birth outcomes are incompletely understood. The estimated number of PTB infants was approximately 15 million in 2010 worldwide, which represented 11% of all live births 11. Preterm birth (<37 weeks of gestation) is the main cause of neonatal death and the second leading cause (after pneumonia) in children under 5 years of age 10. More than 20 million infants worldwide, accounting for 15.5% of all births, are born with LBW, and 95.6% of these babies occurred in developing countries 9, especially in rural areas. As for another adverse birth outcome, LBW (<2500 g) also contributes a lot to infant mortality and childhood morbidity, as well as individual health during the life course 8. In China, CHD is the most prevalent birth defect, accounting for over 10% of cases of infant mortality in 2008 7. Birth defects are present in about 3% of newborns in the USA 6. Congenital anomalies resulted in about 632,000 deaths per year in 2013 down from 751,000 in 1990 5. They are the primary causes of infant mortality, and different disabilities are in developed countries. For example, birth defects, also known as the congenital disorder, are a condition existing at or before birth regardless of cause. As a widely existing health threat, adverse birth outcomes such as birth defects, low birth weight (LBW) and preterm birth (PTB) can produce great disease burden on fetal health status at birth, as well as potential developmental problems in childhood and future the risk of various diseases 2, 3, 4. Maternal and child health is a part of the most important global public health problems, which has been included as a notable part of United Nations Millennium Development Goals 1. The infection during pregnancy is common in Chinese women and might increase the risk of offspring birth defects and low birth weight, especially in younger, lower education, poor pregnant women. The association of birth defect with the infection could be relatively stable but the effect could be mediated by some important factors such as mother’s age, education level and economic level. There was also a significant increase of low birth weight associated with respiratory infections (1.13(1.01–1.27)). We observed increased risks of birth defects with infections, respiratory infections and genitourinary infections during the pregnancy (OR, 1.59 95% CI: 1.21–2.08 OR, 1.44 95% CI: 1.10–1.87 OR, 3.11 95% CI: 1.75–5.54). Of 22916 rural participants, the overall prevalence of infection was about 39.96%. We used PS-matched (1:1) analysis to match participants with infections to participants without infections. The babies born during 2010–2013 and their mothers were selected with a stratified multistage sampling method. The data used here was from a large population-based cross-sectional epidemiological survey on birth defects in Shaanxi province, Northwest China. The purpose of this study is to examine the relationship between infections and birth outcomes in pregnant Chinese women by using propensity score (PS) matching.


 0 kommentar(er)
0 kommentar(er)
